Diabetes Mellitus it is one of the most important pandemics of the XXI century. Sedentary lifestyle, excessive consumption of processed sugars and the obesity have skyrocketed the incidence of this disease worldwide, with an exponential growth of patients who suffer from it year after year.
 Diabetes is a GLOBAL disease that is not limited to just having high blood sugar. The fundamental problem is that in most cases, the diagnosis is delayed in time as the disease goes unnoticed by the patient for a long period and during this period damage has already occurred, which in most cases is irreversible. There is a general decrease in tissue activity, with a drop in the body’s functional reserves, causing “wear and tear” in organs as important as the kidney, retina, peripheral nerves or arteries, also drastically reducing the ability of the immune system to response to infection.
Diabetes is a GLOBAL disease that is not limited to just having high blood sugar. The fundamental problem is that in most cases, the diagnosis is delayed in time as the disease goes unnoticed by the patient for a long period and during this period damage has already occurred, which in most cases is irreversible. There is a general decrease in tissue activity, with a drop in the body’s functional reserves, causing “wear and tear” in organs as important as the kidney, retina, peripheral nerves or arteries, also drastically reducing the ability of the immune system to response to infection.
All these Diabetes conditions make the feet of diabetic patients one of the target organs with the highest risk of suffering complications in the short, medium and long term.
 If you suffer from Diabetes, it is vitally important to carry out a check up, to know the risk your feet have and thus avoid future complications.
If you suffer from Diabetes, it is vitally important to carry out a check up, to know the risk your feet have and thus avoid future complications.
At IVEI – Marbella Vascular Clinic we have a team of experts in Diabetic Foot in each of the areas that this pathology requires. Our main objective in patients with diabetes is the prevention and treatment of foot ulcers, in case they exist, and their possible causes.
ULCER is the most common precursor to AMPUTATION and lengthens the average hospital stay of patients with diabetes by 59%. That is why PREVENTION is fundamental to avoid its appearance.
WHAT IS THE DIABETIC FOOT?
The Diabetic Foot is a complication associated with Diabetes that can appear after years of evolution of the disease or as a consequence of poor control over time..
The main characteristics are loss of sensation in the feet due to nerve involvement and the progressive deterioration of the most distal blood vessels.
- The foot loses the ability to sense pain and temperature, a blister from rubbing with inappropriate footwear or burning sand on the beach can easily go unnoticed.
- If there is an affectation of the circulation, any type of injury will take longer to heal or it will never heal.
- The immune system is altered making it easier for these wounds to become infected and for the infection to spread rapidly.
The biggest complication of a Diabetic Foot is a difficult-to-heal ulcer that can evolve, without proper treatment, into an infection, an amputation and even a real risk to the patient’s life.
What are the symptoms of diabetic foot?
Most of the time the initial signs and symptoms of diabetic foot go unnoticed.
If you are diabetic, you should be alert and consult professionals in the presence of any of the following symptoms:
- Tingling, cramps, loss of strength, pain when walking in the sole of the foot or in the calf.
- Wounds that do not heal.
- Changes in skin color and temperature, including coldness or paleness.
- Changes in the thickness of toenails or spontaneous fall.
WHEN THESE SYMPTOMS DISAPPEAR OR THE PATIENT DOES NOT FEEL PAIN, IT IS INDICATIVE OF THE PRESENCE OF PERIPHERAL NEUROPATHY.
How the Diabetic Foot Evaluation is performed?
All diabetic patients should have an assessment of their feet and their vascular status. The frequency of revisions will depend on the risk degree of each patient.
The diagnosis is made through the following tests:
Neurological tests
Diabetic neuropathy is the most frequent chronic complication of Diabetes Mellitus. With these tests we assess whether there is affectation of superficial sensitivity with the Semmens-Westein monofilament test and deep sensitivity with the tuning fork or bio-tensiometer.
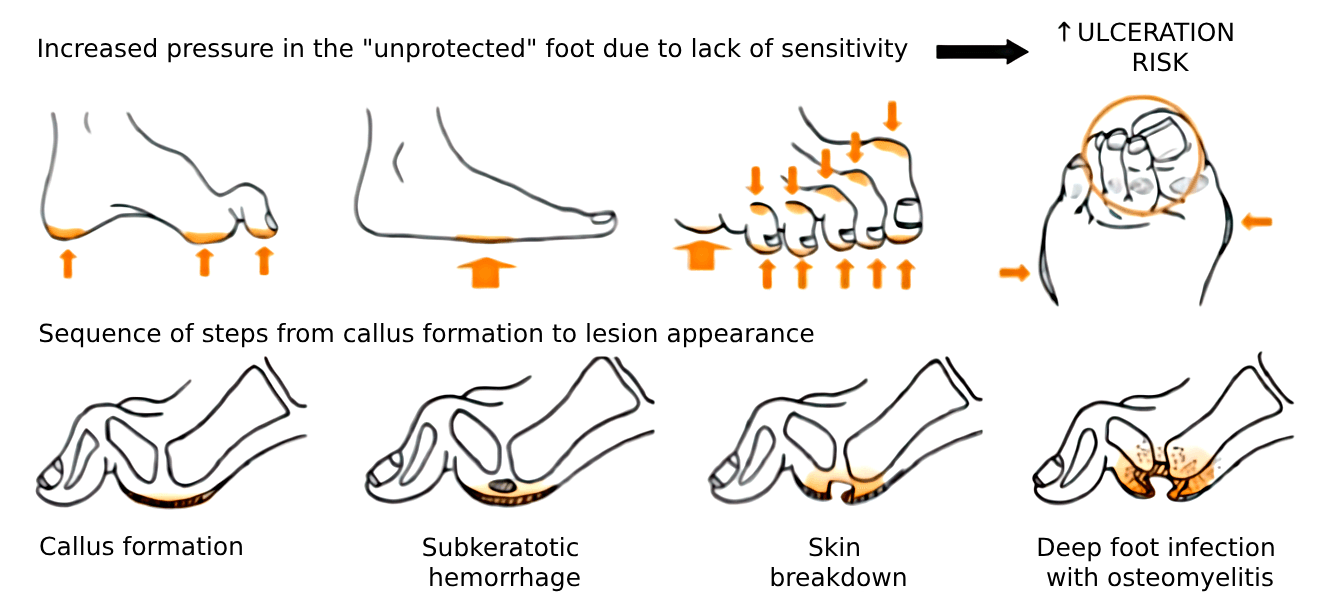
Sensitivity impairment is the main cause of ulceration with subsequent risk of amputation


Foot forms valuation
The presence of deformities increases the risk of developing diabetic foot ulcers..
As a consequence of neuropathy, deformities such as claw toe or bunion, loss of the fat pad or a flattened foot appear. With all this, an increase in pressure occurs and with it, the appearance of calluses..


Vascular tests
Knowing the vascular status of our patient is crucial to be able to know which is the appropriate treatment for him.
For this, different techniques are used such as palpation of distal pulses, the Ankle Brachial Index (ABI), the Pole-test and an arterial Eco-Doppler study if necessary.
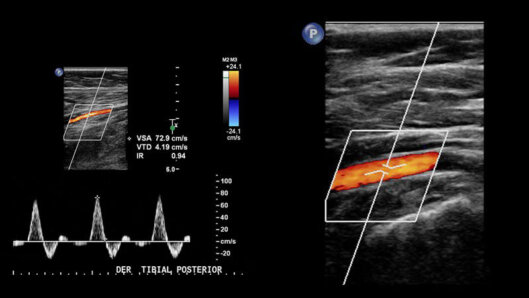

The presence of Peripheral Arterial Disease in a patient with an active foot ulcer conditions a lower probability of healing and an unfavorable evolution.
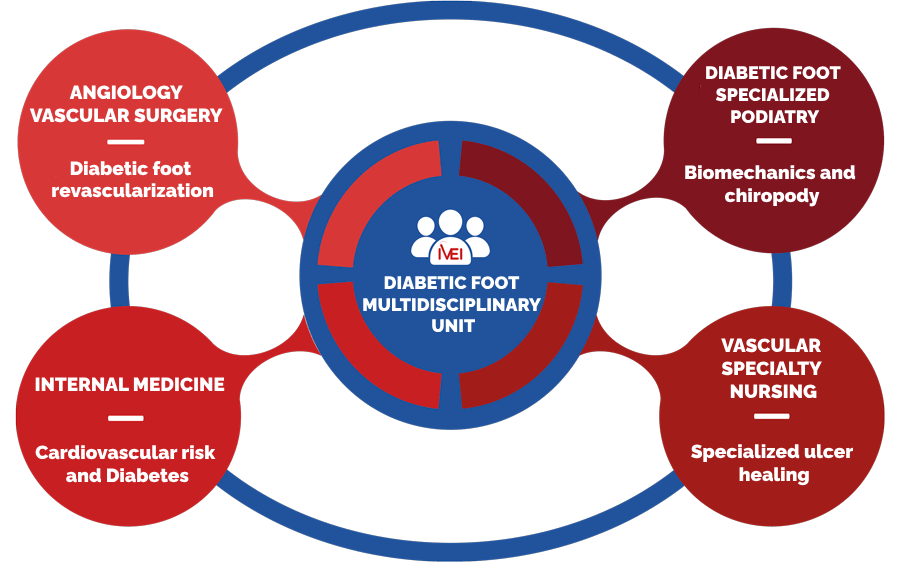
The complexity of diabetic patients requires a multidisciplinary approach to their pathology in order to be successful in their treatment. In the case of Diabetic Foot, the coordinated interaction of Podiatry, Nursing specialized in complex cures and a specialist in Angiology, Vascular and Endovascular surgery is essential for correct and successful management of these patients.
ANGIOLOGY AND VASCULAR SURGERY
Diabetic Foot Revascularization
 Peripheral arterial disease is another of the disastrous consequences of long-standing Diabetes Mellitus. In the case of diabetic patients, the affectation of the arteries below the knee is typical, with the characteristic appearance of calcinosis in the arterial wall and selective involvement of the foot arteries.
Peripheral arterial disease is another of the disastrous consequences of long-standing Diabetes Mellitus. In the case of diabetic patients, the affectation of the arteries below the knee is typical, with the characteristic appearance of calcinosis in the arterial wall and selective involvement of the foot arteries.
In case a diabetic patient presents an ulcer in any of his feet, the evaluation and diagnosis of peripheral arterial disease is essential, since in cases in which it is present, revascularization of the extremity is essential to ensure the adequate healing and avoiding a major amputation, and it takes precedence over any other local therapy.
The neuro-ischemic foot is the worst possible clinical picture that a diabetic patient can present. In these cases the probabilities of amputation are very high.
What symptoms or signs will a diabetic patient with peripheral arterial disease present?
- Feet coldness that worsens in the horizontal position.
- Distal tingling sensation and numbness that worsens in bed.
- Pain in the calves with stiffness when walking.
- Wounds on the feet that do not heal, with a dry and dark appearance and are very painful on handling.
- Loss of distal hair, weakness or even toenail fall.
Given these symptoms, a thorough vascular examination will be essential to establish a diagnosis and an adequate therapeutic plan.
At Marbella Vascular Clinic, our specialists in Angiology, Vascular and Endovascular Surgery are also specialists in minimally invasive procedures to revascularize and reestablish blood flow in diabetic patients with arterial disease. A thorough knowledge of the anatomy and physiology of the foot’s own circulation is essential to achieve correct revascularization aimed at healing injuries and preserving the patient’s limb.
These procedures are performed by selective extremity catheterization. They are performed by puncture, without surgical wounds, with minimal aggressiveness for the patient, a 24-hour hospital stay and practically immediate post-intervention recovery.
DIABETIC FOOT SPECIALIZED PODIATRY
Biomechanics and Chiropody
The key to success in avoiding ulcerations or re-ulcerations in diabetic patients is good foot control, accompanied by an individualized treatment of therapeutic insoles and shoes. Therefore, knowing how your feet work is essential to avoid future injuries.
Footprint study
For this assessment we carry out a complete study of your feet both in loading and unloading. With this we assess the joint mobility of the main joints of the foot and ankle, accompanied by a study of the pressure zones through a digital pressure platform.
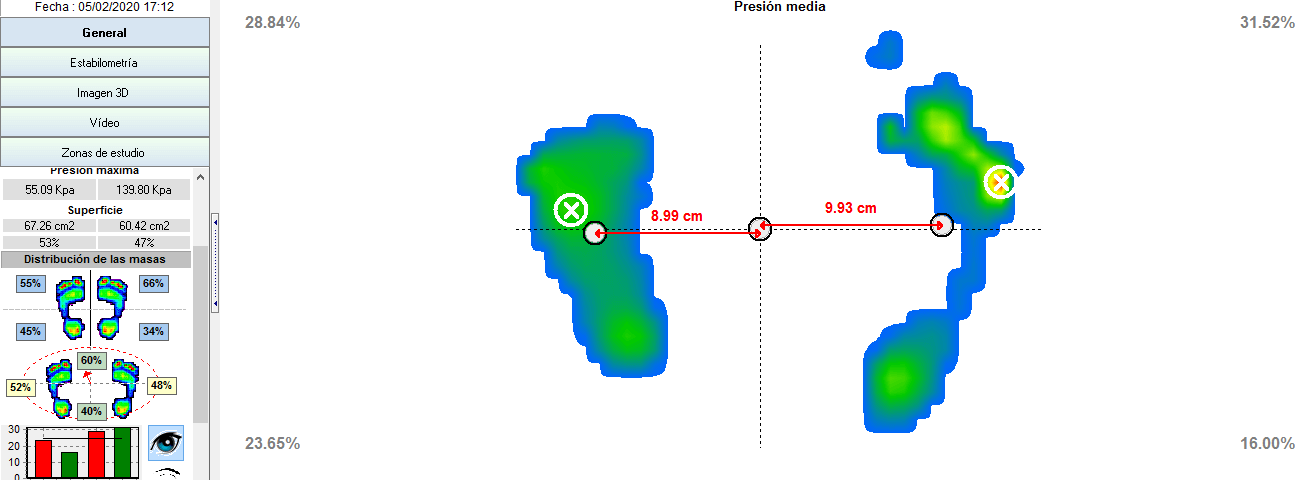
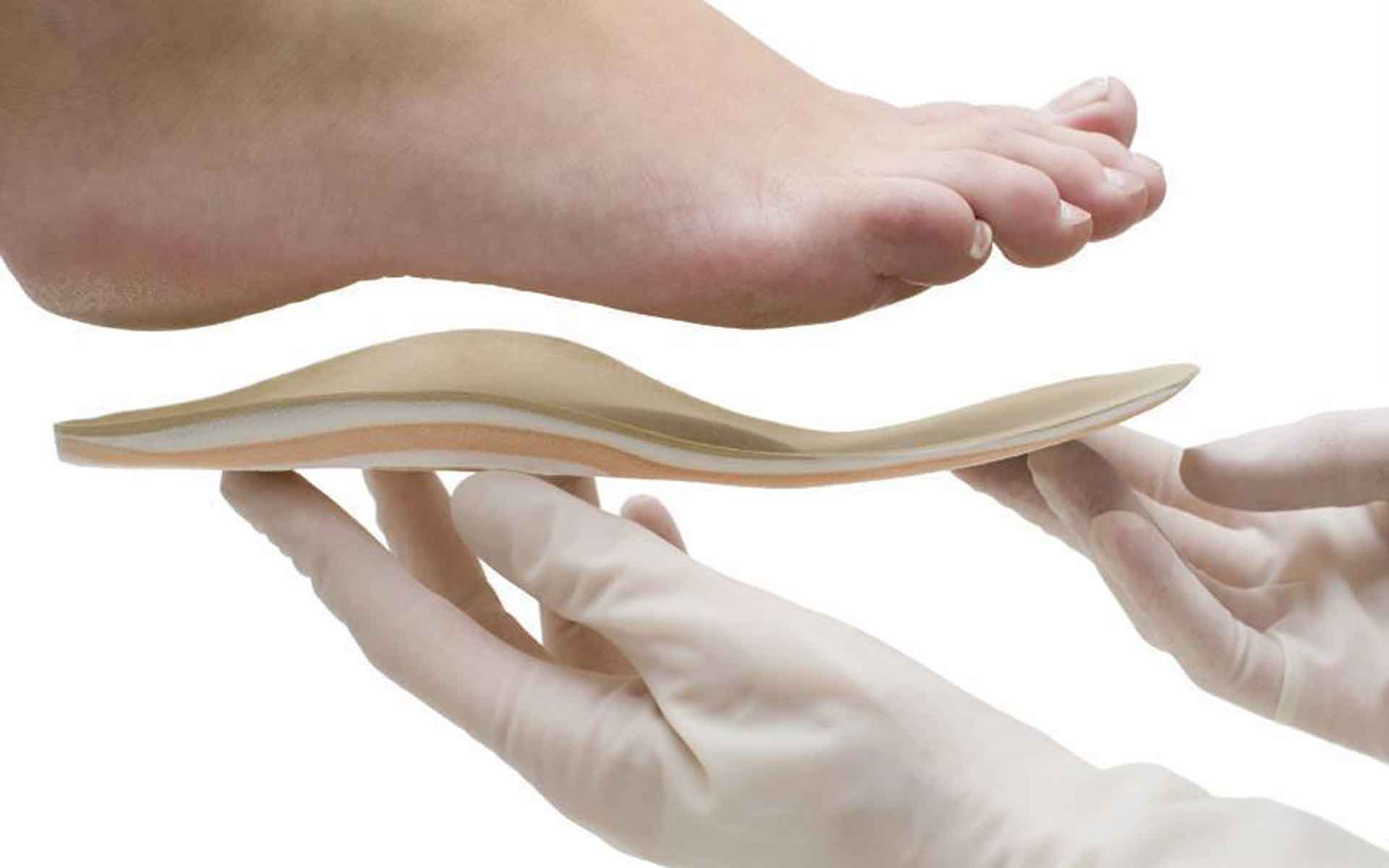
Custom insoles
We make customized and individualized insoles for each patient and always after a biomechanical assessment. The main objectives are to achieve pressure distribution, relieve pressure areas, biomechanical compensation and containment of deformities, in order to prevent ulcerations.
Diabetic foot discharge treatment
En el manejo de las úlceras la reducción de la presión es lo más importante. Las terapias de descargas están diseñadas para reducir la cantidad de presión que recibe el pie en el sitio de la úlcera.
In the management of ulcers, pressure reduction is the most important thing. Offloading therapies are designed to reduce the amount of pressure placed on the foot at the ulcer site.
We offer different types of temporary relief during the ulcer healing process, including felts, post-surgical shoes, and walker boots (Optima ® Boot).

Shoe therapy
Up to 76% of amputations are related to use of inappropiate footware
Therapeutic footwear reduces the incidence of ulcers in people diagnosed with Diabetes Mellitus with foot deformities, compared to regular footwear. The use of therapeutic footwear is essential, with no visible internal seams, lateral buttresses and rigid or semi-rigid biomechanical soles with rockers.


Basic foot care. Chiropody and digital orthosiology
Treatment of calluses that appear on the feet, toenails deseases, such as the presence of fungus or ingrown toenail.
La principal causa de las callosidades o durezas es debido la presión excesiva como consecuencia de una mala pisada o un apoyo patológico o bien por el roce de un calzado inadecuado. Esta presión excesiva puede llevar a la aparición de úlceras en pacientes diabéticos.
The main cause of calluses or hardness is due to excessive pressure as a result of a bad footstep or pathological standing or due to rubbing from inappropriate footwear. This excessive pressure can lead to the appearance of ulcers in diabetic patients.

VASCULAR SPECIALIZED NURSING
Curación Especializada de Úlceras
 We carry out a multidisciplinary approach, with an initial assessment of each patient and patient’s pathology, with the aim of ensuring a correct treatment of it, thus guaranteeing the recovery.
We carry out a multidisciplinary approach, with an initial assessment of each patient and patient’s pathology, with the aim of ensuring a correct treatment of it, thus guaranteeing the recovery.
The main thing in the treatment of a wound is to carry out an exhaustive CLEANING of it, eliminating dead tissues and the edges of the lesion (hardness), since they can interfere with the healing process. In the same way, it is very important to properly TREAT the different tissues that exist in the wound, assess the presence or not of infection and control its exudate. Last but not least, it is necessary to PROTECT the tissues already generated, the perilesional area and the whole of the affected limb.
At the local treatment level we have a wide range of dressings, innovative products and, above all, advanced therapies with the latest technology with the aim of accelerating the healing process and reducing the risk of infection.
Platelet-rich plasma biological therapy
Platelet-rich plasma (PRP) is a platelet concentrate obtained from the patient’s own plasma.
What are the benefits of PRP in the treatment of ulcers?
PRP has the ability to accelerate tissue regeneration, anti-inflammatory effect and decrease the pain. All these processes are key in tissue regeneration and in reducing the recovery process.
How is this therapy performed?
A blood extraction is performed on the patient, similar to that required for a normal analysis. Next, the obtained blood tubes are placed in a centrifuge, in charge of separating the blood cells.

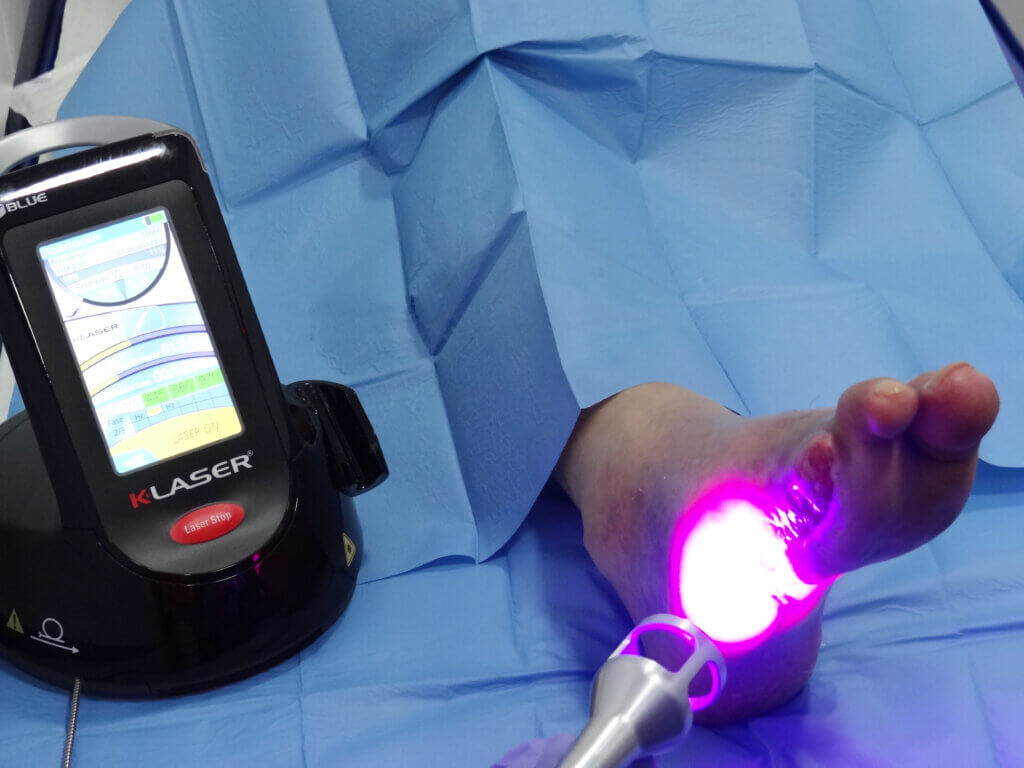
K-Laser Therapy
The application of laser therapy has shown its effectiveness in improving the healing of open ulcers, in reducing pain and in reducing the risk of infection.
What benefits does this therapy provide us in ulcer healing?
The K-Laser Cube improves vascular activity, significantly increasing the formation of new capillaries and vasodilation in damaged tissue, accelerating the healing process and reducing the formation of fibrous tissue.
GREATER BLOOD FLOW EQUALS FASTER HEALING AND LESS PAIN.
Laser light accelerates the process by stimulating the production of fibroblasts in damaged tissue and reduces the formation of scar tissue, which in many cases ends up being a source of chronic pain.
Ozone therapy
What is this therapy?
Ozone therapy consists of the application of a mixture of ozone and oxygen produced by a generator.
What benefits does it bring?
- Regenerative action so that wounds tend to heal faster and accelerated granulation tissues.
- It will remove all bacteriological agents from the wound. In addition, it helps to improve the blood risk of the area to be treated.

Negative Pressure Therapy
What is Negative Pressire Therapy?
Negative Pressure Therapy (NPT) is a type of treatment that promotes the formation of new tissue quickly and safely in order to cover sensitive structures. This therapy is highly indicated in large or deep lesions.
What are the benefits of this therapy in the healing of diabetic foot ulcers??
- Removal of exudate and fluids.
- Preparation of the wound bed in a controlled and closed humid environment.
- Edema reduction.
- Stimulation of angiogenesis by increasing local blood flow, favoring the formation of granulation tissue.
- Reduced infection rates.


